HEPATIC ENCEPHALOPATHY IN THE DOG: MAGNETIC RESONANCE IMAGING AND SPECTROSCOPY (MRS)
Introduction/Purpose
Hepatic encephalopathy is a neuropsychiatric syndrome observed in patients with severe hepatic dysfunction. An abnormal serum levels of substances normally metabolized by the liver normal functioning (ammonia, mercaptans, phenols, short-chain fatty acids) together with glucose and electrolyte imbalances cause an alteration of brain neurons and glia. In Human Medicine has long been known that this syndrome are demonstrable in vivo by magnetic resonance spectroscopy (MRS) of hydrogen. The purpose of this study was to evaluate the cerebral biological compounds using MRS in canine patients with hepatic encephalopathy.
Hepatic encephalopathy is a neuropsychiatric syndrome observed in patients with severe hepatic dysfunction. An abnormal serum levels of substances normally metabolized by the liver normal functioning (ammonia, mercaptans, phenols, short-chain fatty acids) together with glucose and electrolyte imbalances cause an alteration of brain neurons and glia. In Human Medicine has long been known that this syndrome are demonstrable in vivo by magnetic resonance spectroscopy (MRS) of hydrogen. The purpose of this study was to evaluate the cerebral biological compounds using MRS in canine patients with hepatic encephalopathy.
Materials and Methods
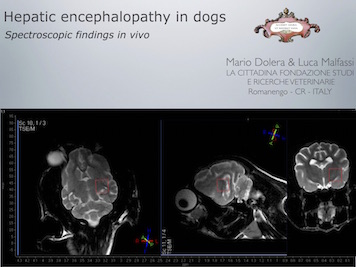
20 dogs with clinical signs of hepatic encephalopathy, were enrolled in this study. The investigation included 1.5T H-MRS with a STEAM single-voxel sequence, TR 244 ms at level of piriform lobe. 10 normal dogs were studied as a control. The spectroscopic findings were correlated to the duration and gravity of clinical symptoms, the morphological MRI findings, the value ammoniemia detected.
20 dogs with clinical signs of hepatic encephalopathy, were enrolled in this study. The investigation included 1.5T H-MRS with a STEAM single-voxel sequence, TR 244 ms at level of piriform lobe. 10 normal dogs were studied as a control. The spectroscopic findings were correlated to the duration and gravity of clinical symptoms, the morphological MRI findings, the value ammoniemia detected.
Results
16 dogs presented congenital portosystemic shunt, 2 microepatia, 1 microangiodisplasy and 1 cirrhosis. The values of ammonia detected ranged between 180 and 340 mcg/dl. All patients showed various degrees of hyperintensity in the gray matter and white matter of the brain in MRI with long TR.
The most commonly MRS results encountered are: increased glutamine-glutamate complex (Gln-GLX/CR: mean 0.40, SD 0.13), decreased choline (CHO/Cr: mean 1.14, SD 0.34), decreased myo-inositol (ml/Cr: mean 0.15, SD 0.08), reduction of n-acetyl-aspartate (NAA: 1.02 average, standard deviation 0.35). These findings in the spectroscopic variations compared to the normal spectrum are greater in patients with high levels of ammonia.
Discussion/Conclusion
The increase in Gln/GLX, the reduction of CHO, NAA and ml may be suggestive of hepatic encephalopathy in dogs. These findings are similar to what is known in human medicine. The safe attribution of a general or neurological symptoms to liver dysfunction associated with hepatic encephalopathy may be difficult to implement by the clinician. The authors believe that the arguments deserve further study to evaluate the quantitative analysis of changes in metabolities as a function of duration of the symptoms.
16 dogs presented congenital portosystemic shunt, 2 microepatia, 1 microangiodisplasy and 1 cirrhosis. The values of ammonia detected ranged between 180 and 340 mcg/dl. All patients showed various degrees of hyperintensity in the gray matter and white matter of the brain in MRI with long TR.
The most commonly MRS results encountered are: increased glutamine-glutamate complex (Gln-GLX/CR: mean 0.40, SD 0.13), decreased choline (CHO/Cr: mean 1.14, SD 0.34), decreased myo-inositol (ml/Cr: mean 0.15, SD 0.08), reduction of n-acetyl-aspartate (NAA: 1.02 average, standard deviation 0.35). These findings in the spectroscopic variations compared to the normal spectrum are greater in patients with high levels of ammonia.
Discussion/Conclusion
The increase in Gln/GLX, the reduction of CHO, NAA and ml may be suggestive of hepatic encephalopathy in dogs. These findings are similar to what is known in human medicine. The safe attribution of a general or neurological symptoms to liver dysfunction associated with hepatic encephalopathy may be difficult to implement by the clinician. The authors believe that the arguments deserve further study to evaluate the quantitative analysis of changes in metabolities as a function of duration of the symptoms.